©2025 Copyright Innergarden Health • All rights reserved • Website by AtefDesign

If you don’t know much, or anything, about Bacterial BioFilm, you’re not alone. Even top health and medical experts mostly have no idea of what they are, much less that they are considered the Number One reason why many known medical and natural protocols simple don’t work, and when they do calm symptoms temporarily, why people relapse.
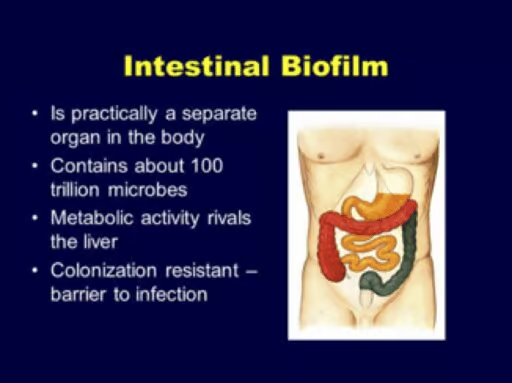
In this research article I share with you a few facts on the intestinal microbiome and why researchers are now developing more studies.
 Biofilm formation occurs when free-floating microorganisms attach themselves to a surface, as in the wall of the intestines, and create a colony.
Biofilm formation occurs when free-floating microorganisms attach themselves to a surface, as in the wall of the intestines, and create a colony.
They secrete materials (extracellular polymers) that provide a structural matrix that adheres to surfaces.
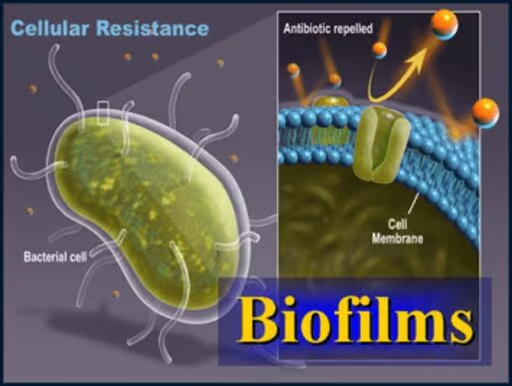
Because biofilms protect the bacteria, infections are often more resistant to traditional antimicrobial treatments, making them a serious health risk.
Biofilm bacteria generally tolerate antibiotic and antifungal treatment because antibiotics cannot pass through the biofilm – it’s like an armor protecting the bacteria[1].
Biofilms are known to be involved in many chronic infections such as in a chronic wound, lung, ear, heart, and nose infections[2].
Studies show that up to 59% of people with chronic sinus infections were found to have a bacterial biofilm, whereas none of the controls (people who did not have a sinus infection) had bacterial biofilm[3].
The most common biofilm you might be familiar with is the plaque on your teeth[4].
Biofilm is a toxic, sticky plaque that bacteria & yeast secrete, which acts as a blanket within the body where they can hide out and multiply.
AND…biofilm is everywhere, especially in the intestinal tract, and continues to attach and protect itself as it multiplies and creates more biofilm. In one study, medical researchers found that bacteria hidden underneath biofilms were up to 1,000x’s more likely to survive even the most potent antibiotics . And biofilm is also the #1 reason why we are suddenly seeing a huge rise in the drug-resistant bacteria showing up in the world – not to mention the overuse of antibiotics.
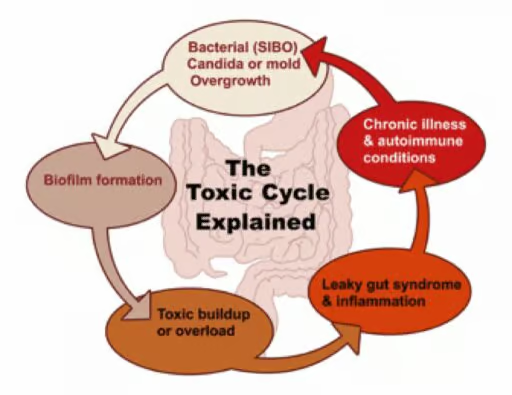
Once biofilm becomes established in the body, these harmful bugs are free to multiply under the safe layer of this biofilm plaque.
The more these bugs populate beneath their biofilms, the more bio-waste ends up accumulating within the body, reaching a critical-mass. Once this mass is reached, a chain-reaction of events begins taking place in the body as it becomes increasingly compromised.
AND…all of this starts in the gut!
Never before has there been more research pouring into this subject than right now. Experts agree that, “after all, if our bodies are more microorganisms than human, wouldn’t it make sense to pay close attention to our microbiome for answers?”
Currently there is compelling evidence that over 80% of individuals dealing with a chronic condition are actually experiencing some form of microbial or yeast overgrowth as the underlying cause. [5]
The four main “bugs”, or health-depleting microbes, most people suffer from are bacteria, yeast, parasites & molds.
One of the most challenging factors with microbial overgrowth’s is that they are often responsible for long-term health symptoms such as, but not limited to: body aches, mood and sleep disorders, poor digestion, blood sugar disorders, chronic migraines, kidney disorders, compromised immunity, brain-fog and extreme lethargy.
 BioFilm’s “Blueprint” for Survival
BioFilm’s “Blueprint” for SurvivalThe BioFilm “war plan,” for survival as populations mature, is to become resistant to even the toughest treatment protocols – and that is very evident as more and more reoccurrences emerge after the initial condition is either under control or eradicated via dietary modifications and supplementation and/or anti-fungal medications.
In the body, when biofilms form, they create a protective layer by which bacteria evade the immune system and antimicrobials in order to continue their toxic cycle.
Bacteria become tolerant to antibiotics and most other antimicrobial agents.
So if you have a fungal or bacterial infection that is coated with a biofilm, one theory suggests that normal antibiotics and antifungals will not kill the infection.
If you have a bacterial infection that persists despite antifungal therapy and you have a high level of proinflammatory cytokines, some scientists believe this implies that you either have a biofilm or a non-bacterial infection.
When bacteria form biofilms, they do not lump together by chance. In order to form biofilms, bacteria need to communicate with each other[6].
One way to disrupt biofilm formation is to interrupt bacterial communication, also known in science as quorum sensing (QS).
The following items known to be communication disruptors are listed strictly for educational purposes as indicated by recent research and not meant in any way to indicate a diagnosis, treatment, or cure:
FOODS
Non-Herbal Biofilm Disruptors
ENZYMES
HERBAL BIOFILM DISRUPTORS
END NOTES:
It has been my experience that a considerable amount of biofilm is expelled as part of a colon therapy session and is usually mixed with excess mucous that often is seen as large “chunks” of gelatinous waste.
213 + 214-2190 Fir St.
Vancouver, BC, V6J 3B5
located in Afrina Beauty,Spa, & Health
140 – 700 Marine Drive
North Vancouver, BC
Sign up for our mailing list to receive our monthly newsletter
and any future promotions.
We are grateful to be working and residing on the unceded territories of the Coast Salish peoples, including the Sḵwx̱wú7mesh (Squamish), Stó:lō and Səl̓ílwətaʔ/Selilwitulh (Tsleil-Waututh) and xʷməθkʷəy̓əm (Musqueam) Nations.
Last Minute Same Day Special! Book for today any 60 or 75 minute session – $40 off. Cannot be combined with any other offer. Use promo code: Save40